Social Care: Is Artificial Intelligence the answer when current processes are not very Intelligent at all. (Silver bullet or a blank?)
The Tale of the Golden Generation
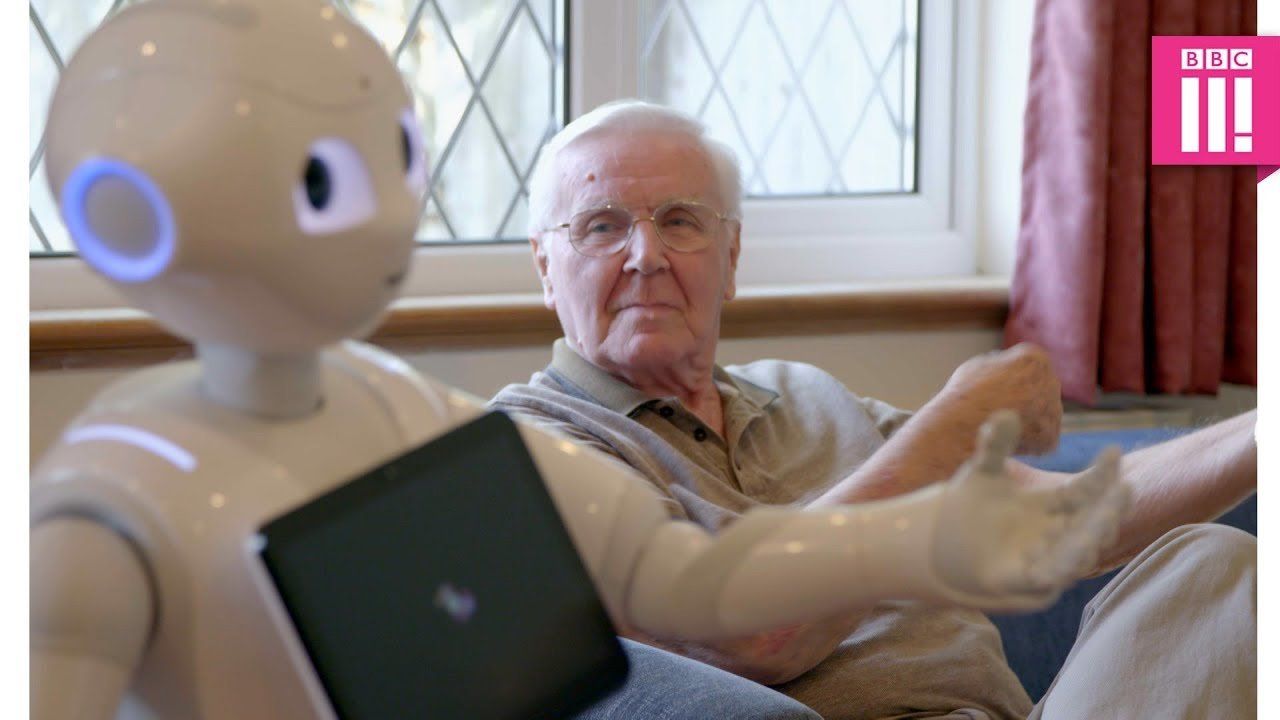
I must admit I do fear for Artificial Intelligence in the world of Social Care, and yet what it can do is impressive. For some it will be a godsend and will bring life changing aspects to their quality of life, but alas I believe that this will be for the fortunate few and not the many.
Despite the hype it reminds me a little of England’s Golden Generation of footballers. The abundance of potential talent looked like it would be the answer to all England supporters’ dreams, all those years of hurt etc. but in fact it never quite worked, and no one ever really could explain why. I guess that players got injured, they never worked together as expected and the challenges that they faced (the other teams) also changed. In a similar way the potential of AI looks impressive, but I fear other forces will overwhelm it as the silver bullet that will solve the Social Care puzzle. I genuinely hope I am wrong and do believe that it will help but the scale of the challenge feels insurmountable when you look at the current problems.
The examples that you see on social media are in some instances fantastic, but they are not a magic wand, and will they solve the problems that they are up against. The AI may well be a strong swimmer but the tide it is swimming against would seem to be of a far greater force.
The Knowns – Demand going up and the number of trained carers going down
The facts are quite simple as there is an unprecedented growth in the percentage of aging population throughout the world, particularly in growing economies such as Europe, Japan and China, something that we in the UK rarely give any thought to.
I read last week that from 2000 to 2050, the percentage of the world’s population who is 60 years of age and older is estimated to approximately double from about 12% to 22% (from 605 million to 2 billion).
This rapid aging demographic will directly affect social, economic and health outcomes for these growing economies. How will such demands be met, keeping in mind the prevalence of chronic diseases and the requirements of the elderly and geriatric patients. Geriatric diseases such as osteoporosis, cardiovascular diseases, obesity, diabetes, dementia and osteoarthritis require quick diagnosis and continuous supervision by a professional caregiver.
This is coupled with the fact that we are not training enough Doctors and carers to account for the increased demands of healthcare. The problems are obvious, but the solutions are not.
Given the situation, healthcare providers are starting to offload certain parts of the care-pathways to artificial intelligence (AI). AI can now be found in healthcare, starting from intelligent tracking of biometric information to early diagnosis of diseases. AI is helping patients and their families understand the treatment pathways. AI is also helping clinicians to treat the conditions more efficiently.
Artificial intelligence is a key component of the future of healthcare. Indeed, the era of the AI doctor seems to be unavoidable. Today, we see AI in hospitals helping clinicians identify medical risks; predict when to provide targeted, life-saving interventions; form treatment plans for patients with rare diseases; and deliver precision medicine.
However, this is AI being used mainly in a medical environment and by professional staff, where it is fully resourced and professionally managed, however the care at home scenario is somewhat different, where to a certain degree much of it will be managed remotely, which in itself will bring many challenges. The other challenge faced is that the elderly cared for at this point in time are not “IT friendly”. This is a fact that cannot really be changed but will hopefully reduce as an issue as the IT generation become the users.
My cynicism is unfortunately born out of experience and knowledge of the sector. The quality and available resources for administrative support for most businesses is generally poor and therefore the chances of the theory becoming reality are somewhat limited as implementation and ongoing maintenance will create challenges that will be very difficult to maintain. In addition to this the question of potential liability may become an issue for providers, as if you have systems with alerts and warnings and these are not acted upon then there may be a potential liability due to the inaction. If this was to be the case then what funding would be needed to fully support such a system with adequately trained staff 24 hours a day, 7 days a week.
The historical underfunding of the sector pervades throughout the businesses, from the inability to recruit carers at or around minimum pay levels to the resources available to administer and support the day to day business. Funding has been and will remain the key issue to the Care crisis.
At one of the National Care Shows several months ago I bumped into a former colleague who now is the CEO of one of the Care Sectors largest providers of Care Management software. Whilst I appreciate that Care Management software is not AI the conversation that we had painted a picture of the challenge to be faced by introducing change into the care system. Following a brief chat about how we managed 25 years ago he gave me a great insight into where the Care Home Management systems market is today and what the modern cloud-based solutions can offer. I was impressed, and it all made sense. Easy to use, safe, GDPR compliant and appeared to be affordable. The solutions are on a single platform and are integrated and relatively easy to use, and in a care home environment can be controlled well.
Now that all made sense to me, however he then told me that only in the region of 10% to 12% of all care homes use such systems and the rest still rely on antiquated or in many cases paper-based systems with historical processes that are not integrated. Being honest I was initially shocked but having time to think about it afterwards I thought that I should not really be shocked. If you then bear in mind that Domiciliary care businesses are more difficult to manage due to the remote nature of the client base and the workforce, then introducing change will be even more difficult.
In the last 6 months I have spent a great deal of time looking at the Care Management solutions for Domiciliary, Complexed and Supported Living care, and whilst as ever in the wake of the Care Home sector, the products are developing quickly. However, the greatest hurdle is not financial, as the solutions are now affordable, but it is the reluctance to change and the lack of resources to enable successful implementation, a message clearly echoed from the Care Home sector.
If you then consider the introduction of a new generation of technology into social care, then it is not all about robots I’m afraid because somewhere in the process there are still going to be a lot of humans.
Phil Talbot is a Chartered Accountant and Business Consultant, specialising in the provision of business and accounting advice for small business offering part-time FD services.
With over 26 years in Senior Finance roles including 16 years as Finance Director in one of the UK’s largest and most successful Social Care Business he has specialist knowledge and experience of the Health and Social Care Sector. Any businesses interested in Non-Executive Director Support, advice with regards to Care Management systems or part time FD Support then please contact.
email : phil.talbot@pjtconsultancy.co.uk
Phone : 07967 640082
���